Intrauterine Adhesions (Asherman Syndrome): A Cause for Concern in Infertility and Recurrent Miscarriage
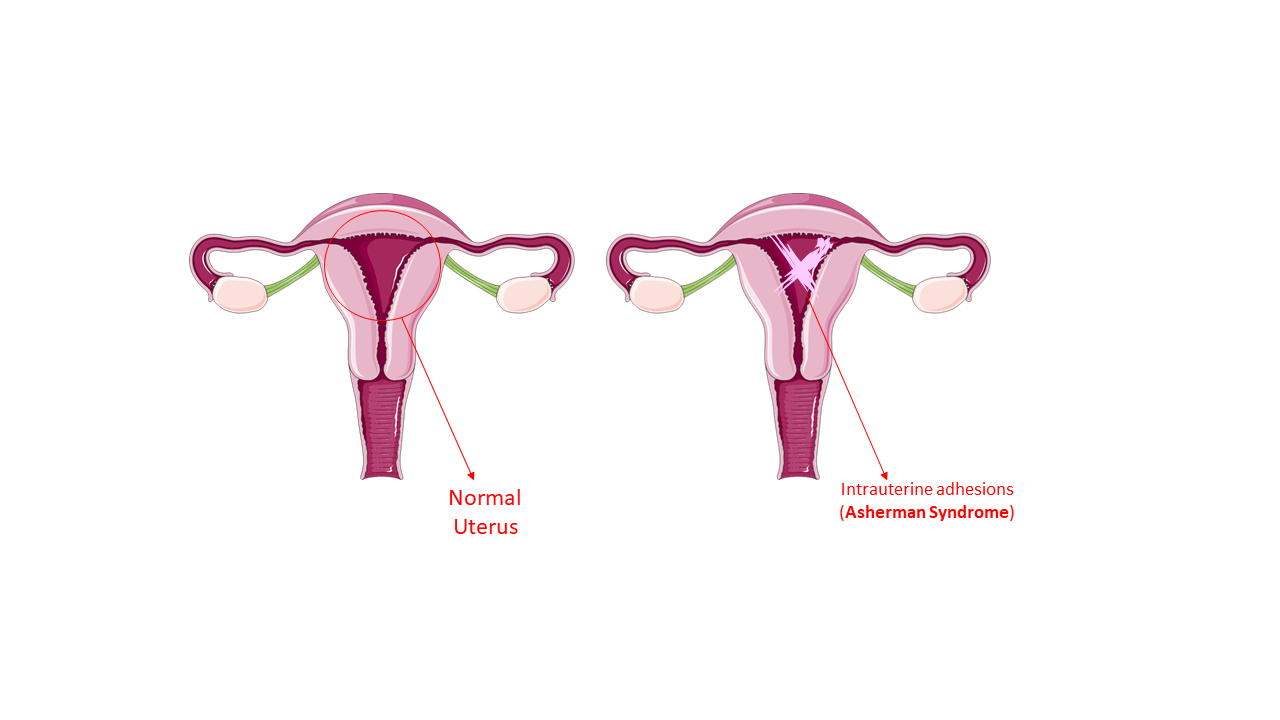
Intrauterine adhesion, or synechiae, is an acquired uterine condition characterized by the formation of scar tissue between the inner walls of the uterus and/or cervix, causing the walls to abnormally adhere to each other.
Asherman syndrome is a term used to describe the adhesions inside the uterus. These adhesions can range in severity from thin and web-like to thick bands of tissue. In severe cases, the uterine cavity may be partially or completely occluded when the walls of the uterus and/or cervix fuse together.
How Does Asherman Syndrome Affect Fertility?
It may be difficult for you to become pregnant if you have Asherman syndrome. If you do, your chances of having a miscarriage are high. It is possible to become pregnant while suffering from the syndrome, but the adhesions in the uterine walls prevent fetal development. This increases your chances of having a miscarriage or stillbirth compared to women who do not have the syndrome.
Asherman syndrome also increases the risk of certain pregnancy complications, such as:
- Placenta accreta. The placenta protrudes too deeply into the walls of the uterus. This results in a high-risk pregnancy. After birth, all or part of it remains attached, resulting in excessive bleeding.
- Placenta Previa. The placenta blocks the cervical opening, causing severe bleeding during pregnancy and birth. It also increases the risk of premature delivery.
- Excessive bleeding. It can cause miscarriage, infection, or be a sign of an ectopic pregnancy. An ectopic pregnancy is one that occurs in your fallopian tube.
Asherman syndrome is not a life-threatening condition, but it might expose you to recurrent miscarriages. If you have Asherman syndrome, make sure you see your doctor on a regular basis so that they can monitor your pregnancy.
Causes of Asherman Syndrome
Intrauterine adhesions are usually caused by damage to the uterine tissue; however, sometimes the precise cause of the adhesions is unknown. The most common cause of intrauterine adhesions is injury to the uterine cavity during a surgical procedure.
Here’s a list of the known causes of Asherman syndrome:
- Dilation and curettage (D&C) following an elective abortion procedure, a miscarriage, or the removal of a retained placenta after delivery.
- Infections of the uterine lining (endometritis),
- Surgical procedures such as a myomectomy
- Cesarean sections
- Endometrial ablation, a surgical procedure that is used to intentionally damage the uterine lining to make menstrual periods lighter or eliminate them entirely.
- Endometrial tuberculosis.
Symptoms of Asherman Syndrome
A woman with intrauterine adhesions may experience no obvious symptoms. However, some women may experience the following symptoms:
- menstrual abnormalities such as absent, light, or infrequent periods
- painful menstrual periods.
- inability to achieve pregnancy or recurrent miscarriages
- pelvic pain
Diagnosis of Asherman Syndrome
Hysteroscopy, Hysterosalpingogram (HSG), or Saline Sonohysterogram (SHG) can all be used to diagnose Asherman syndrome. Hysteroscopy is the most accurate method of diagnosing and evaluating intrauterine adhesions.
It is a procedure in which a thin, lighted telescope-like instrument is inserted through the cervix to directly visualize the uterus.
Treatment of Asherman Syndrome
The most common treatment for Asherman syndrome is hysteroscopic surgery. A hysteroscope is used to cut the scar tissue. This procedure is usually done under anesthesia.
After cutting off the adhesions, it is recommended to temporarily place a device, such as an IUCD, a plastic catheter, or a balloon inside the uterus to keep the walls of the uterus apart and to minimize the likelihood of adhesions reforming.
After the procedure, hormonal therapy with estrogen and sometimes NSAIDs and/or antibiotics is often prescribed to further reduce the likelihood of adhesions reforming. In severe cases, it may be necessary to have more than one surgery to remove adhesions.
Do I need to worry about any issues after treatment?
Some patients continue to experience absent or infrequent periods even after receiving treatment.
Miscarriage, preterm labor, third-trimester bleeding, and/or abnormal placental attachment to the uterine wall are more likely to complicate pregnancies that develop after treatment. The type and severity of the adhesions correlate with the likelihood of a successful pregnancy following treatment.
Patients with mild to moderate adhesions typically regain normal menstrual function following treatment, and their chances of conceiving successfully at full term range from 70% to 80%.
In contrast, patients with severe adhesions or significant endometrial lining damage may experience full-term pregnancy rates of only 20% to 40% or lower following treatment.
Women who have extensive endometrial damage that does not improve after treatment may consider adoption or in vitro fertilization (IVF) using a “gestational carrier,” in which another woman carries the pregnancy for the mother using the patient’s eggs.
At Primecare Fertility Clinic, we provide excellent IVF services, including IVF with a gestational carrier. So regardless of the outcome of your treatment, we’ve got you covered. Contact us today, and our specialists will advise you on the next steps to take.
ReferenceS
“What Is Asherman Syndrome?” WebMD, 28 May 2021, www.webmd.com/women/what-is-asherman-syndrome.
“Intrauterine Adhesions: What Are They?” Reproductive Facts, www.reproductivefacts.org/news-and-publications/patient-fact-sheets-and-booklets/documents/fact-sheets-and-info-booklets/intrauterine-adhesions-what-are-they. Accessed 10 Dec. 2022.
Add Your Comment